Upper cervical chiropractic care addresses vertigo and dizziness by correcting misalignments in the atlas (C1) and axis (C2) vertebrae that can disrupt the vestibular system and brainstem function.
Studies show 60-85% of vertigo patients experience significant improvement with upper cervical adjustments, particularly for cervicogenic vertigo and post-concussion dizziness.
By downloading the Digital Patient Chart mobile app you can better control your patient portal.
Affects: 40% of adults experience vertigo at least once in their lifetime
Causes: Upper cervical misalignment, inner ear disorders, vestibular dysfunction, head trauma
Success Rate: 60-85% improvement with upper cervical care for appropriate cases
Recovery Timeline: Most patients notice improvement within 4-8 sessions
Vertigo isn't just feeling lightheaded, it's a distinct sensation that you or your surroundings are spinning, tilting, or moving when they're actually still. For the millions who experience this disorienting condition, it can severely impact daily life, from driving and working to simply getting out of bed.
While many people associate vertigo solely with inner ear problems, emerging research reveals that issues in the upper cervical spine, specifically the top two vertebrae of your neck, may be a significant but often overlooked contributor. Upper cervical chiropractic care, particularly the Blair technique, offers a precise, gentle approach that addresses vertigo at its neurological source.
This content is for informational purposes only and does not constitute medical advice. The information provided should not be used for diagnosing or treating health problems or diseases. Always consult with a qualified healthcare provider before making any healthcare decisions or for guidance about specific medical conditions.
What Is Vertigo?
Vertigo is a specific type of dizziness characterized by a false sensation of movement—either you feel like you're spinning, or the room appears to be spinning around you.
Unlike general lightheadedness or feeling faint, vertigo involves a rotational component that can range from mild and brief to severe and debilitating.
The condition affects the vestibular system, which includes structures in your inner ear and connections to your brainstem that help maintain balance, spatial orientation, and coordinate movement.
When this system malfunctions, your brain receives conflicting information about your body's position and movement, resulting in that characteristic spinning sensation.
Vertigo episodes can last anywhere from a few seconds to several days. Some people experience isolated incidents, while others suffer from chronic, recurring vertigo that significantly diminishes their quality of life.
The severity can range from a mild sense of unsteadiness to intense spinning that triggers nausea, vomiting, and an inability to stand or walk.
There are two main categories of vertigo: peripheral vertigo, which originates from problems in the inner ear or vestibular nerve, and central vertigo, which stems from issues in the brain or brainstem.
However, there's a third, often-missed category: cervicogenic vertigo, which originates from problems in the cervical spine, particularly the upper neck region.
The Upper Cervical Connection
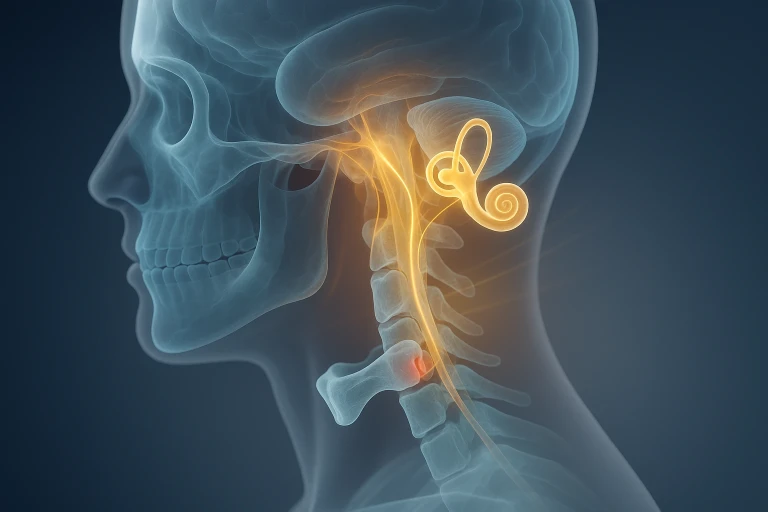
The relationship between the upper cervical spine and vertigo is based on critical anatomical and neurological connections. The atlas (C1) and axis (C2) vertebrae, the top two bones in your neck, have a unique and profound influence on the vestibular system and overall balance function.
Anatomical Proximity to the Brainstem
The atlas vertebra forms a protective ring around the brainstem, where vital balance centers are located.
When the atlas is misaligned, even by millimeters, it can create mechanical stress on the brainstem and disrupt signals traveling between your inner ear balance organs and your brain. This disruption can manifest as vertigo, dizziness, or balance problems.
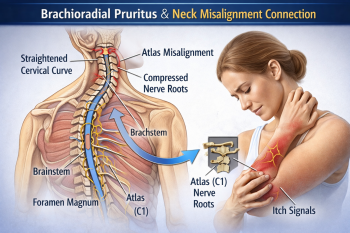
Proprioceptive Input
The upper cervical spine contains an exceptionally high density of proprioceptors—specialized nerve endings that provide your brain with information about head and neck position.
In fact, the upper cervical muscles have more proprioceptors per gram than any other muscles in the human body. When upper cervical alignment is compromised, these proprioceptors can send distorted signals to the brain, creating a sensory mismatch that results in vertigo.
Vertebral Artery Considerations
The vertebral arteries, which supply blood to the posterior brain (including balance centers), travel through small openings in the cervical vertebrae called the transverse foramina.
Upper cervical misalignment can potentially affect blood flow through these arteries, though this is more relevant in extreme cases. More commonly, the issue involves nerve and proprioceptive interference rather than vascular compression.
Vestibular Nerve Connections
The vestibular nuclei in the brainstem receive input from both the inner ear and the upper cervical spine. These nuclei integrate information from multiple sources to create your sense of balance and spatial orientation.
When there's a mismatch between inner ear signals and cervical proprioceptive information, often due to upper cervical misalignment, the brain struggles to determine accurate positioning, resulting in vertigo.
What Causes Cervicogenic Vertigo?
Cervicogenic vertigo specifically refers to dizziness and balance problems originating from the cervical spine. Understanding the causes helps identify whether upper cervical chiropractic care may be an appropriate treatment option.
Whiplash and Auto Accidents
Motor vehicle accidents are among the most common causes of upper cervical misalignment leading to vertigo. The sudden acceleration-deceleration forces of whiplash can shift the atlas and axis vertebrae out of their normal position.
Research indicates that up to 50% of people who experience whiplash develop vertigo or dizziness as a persistent symptom, sometimes appearing weeks or months after the initial injury.
Head Trauma and Concussions
Even seemingly minor head injuries can cause upper cervical misalignment. Falls, sports injuries, and other impacts to the head often transmit force through the skull to the upper neck.
Post-concussion vertigo affects approximately 30-65% of people who sustain a concussion, and upper cervical involvement is frequently a contributing factor.
Chronic Poor Posture
The modern epidemic of "tech neck", forward head posture from prolonged computer, tablet, and smartphone use, creates chronic stress on the upper cervical spine.
Over time, this postural strain can lead to atlas and axis subluxation (misalignment), gradually affecting vestibular function and contributing to balance problems.
Birth Trauma
Surprisingly, upper cervical misalignment can occur during the birth process itself. Difficult deliveries, forceps or vacuum assistance, and rapid delivery can all place significant stress on an infant's neck.
While many people associate chiropractic care with adults, some vertigo cases have roots in birth trauma that went unaddressed for years or decades.
Previous Injuries
Old injuries, even from childhood, can create lasting upper cervical instability. A fall from a bicycle at age 10, a sports injury in high school, or a slip on ice years ago, any of these can create misalignment patterns that eventually manifest as vertigo later in life when additional stress or aging factors come into play.
Degenerative Changes
Arthritis, disc degeneration, and other age-related changes in the cervical spine can alter normal upper cervical alignment and function.
While these changes don't always cause symptoms, they can create conditions where the vestibular system becomes more vulnerable to dysfunction.
Signs and Symptoms
Cervicogenic vertigo presents with a characteristic pattern of symptoms that can help distinguish it from other causes of dizziness. Recognizing these patterns is essential for seeking appropriate care.
Primary Symptoms:
The hallmark symptom is vertigo—a spinning or rotational sensation—that's often triggered or worsened by neck movement or specific head positions.
Unlike inner ear vertigo, which can occur spontaneously, cervicogenic vertigo typically has a clear relationship to neck posture or movement.
Associated Symptoms May Include:
- Neck pain or stiffness, particularly in the upper neck region just below the skull
- Headaches, often starting at the base of the skull and radiating forward
- Visual disturbances such as blurred vision, difficulty focusing, or sensitivity to light
- Nausea and sometimes vomiting, especially during severe vertigo episodes
- Balance problems and unsteadiness, even when not experiencing active spinning
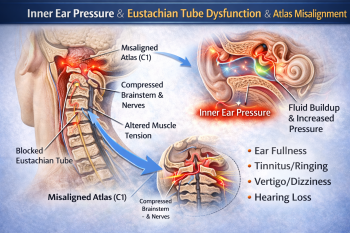
- Tinnitus (ringing in the ears) or a feeling of fullness in the ears
- Cognitive difficulties including brain fog, difficulty concentrating, or memory problems
- Fatigue and anxiety, often related to the unpredictability of vertigo episodes
Symptom Patterns That Suggest Cervicogenic Vertigo:
Several patterns strongly indicate an upper cervical origin:
- Position-dependent symptoms: Vertigo that occurs or worsens with specific neck positions or movements
- History of neck trauma: Even injuries that occurred years ago
- Unilateral symptoms: Dizziness, ear fullness, or tinnitus predominantly on one side
- Relief with certain positions: Finding that specific head or neck positions reduce symptoms
- Combination with neck pain: Vertigo accompanied by upper neck pain or headaches
- Failed inner ear treatments: Little or no response to medications or vestibular rehabilitation designed for inner ear problems
Symptom Progression:
Cervicogenic vertigo may start subtly, with brief episodes of mild unsteadiness or a "foggy" feeling. Over time, episodes may become more frequent, longer-lasting, or more severe.
Some people experience constant low-grade dizziness punctuated by acute vertigo attacks, while others have unpredictable episodes with symptom-free periods in between.
SEEK IMMEDIATE MEDICAL ATTENTION IF YOU EXPERIENCE:
- Sudden, severe vertigo with intense headache (especially "worst headache of your life")
- Vertigo accompanied by weakness, numbness, or paralysis
- Difficulty speaking, vision changes, or confusion
- Loss of consciousness
- Vertigo with chest pain or difficulty breathing
- Signs of stroke (facial drooping, arm weakness, speech difficulty)
These symptoms may indicate serious conditions requiring emergency evaluation rather than upper cervical misalignment.
How Is Vertigo Diagnosed?
Accurate diagnosis is crucial because vertigo can stem from multiple causes, and treatment effectiveness depends on identifying the correct underlying issue. A comprehensive evaluation for vertigo typically involves several steps.
Medical History and Symptom Analysis
Your healthcare provider will ask detailed questions about your vertigo episodes: when they started, how long they last, what triggers them, and what other symptoms accompany them.
Information about past injuries, accidents, or trauma, even from years ago, is particularly relevant for identifying potential upper cervical involvement.
Physical Examination
A thorough physical exam includes neurological testing, evaluation of balance and coordination, eye movement assessments, and cervical spine examination.
Upper cervical chiropractors trained in the Blair technique perform specialized orthopedic and neurological tests to identify atlas and axis misalignment and its effects on the nervous system.
Imaging Studies
Precision X-rays: Upper cervical specialists use specific x-ray views that show the exact position of the atlas and axis in three dimensions.
Blair technique practitioners take images in multiple angles to measure misalignment with millimeter precision. These aren't standard neck x-rays, they're specialized views that reveal the unique anatomy of each person's upper cervical spine.
MRI or CT scans may be ordered to rule out structural problems, tumors, or other central nervous system issues that could cause vertigo. These imaging studies are particularly important when symptoms are severe, progressive, or accompanied by other neurological signs.
Distinguishing between different vertigo causes is essential:
- Benign Paroxysmal Positional Vertigo (BPPV): Caused by calcium crystals in the inner ear canals
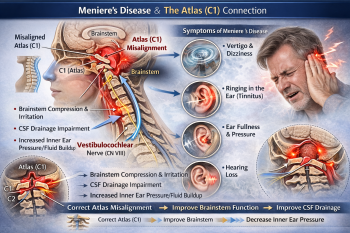
- Ménière's disease: Inner ear disorder causing vertigo, hearing loss, and tinnitus
- Vestibular neuritis: Inflammation of the vestibular nerve
- Central vertigo: Brain or brainstem disorders
- Cervicogenic vertigo: Upper cervical spine dysfunction
- Blood pressure checks, cardiovascular evaluation, and medication review also help rule out other dizziness causes.
The key is that cervicogenic vertigo often coexists with other conditions, and upper cervical correction may improve symptoms even when multiple factors are present.
Upper Cervical Treatment for Vertigo
Upper cervical chiropractic care for vertigo focuses on identifying and correcting specific misalignments in the atlas and axis vertebrae.
This approach differs significantly from general chiropractic adjustments and mainstream medical treatments for vertigo.
The Blair Technique Approach
The Blair technique is a specialized upper cervical method that uses precision imaging and gentle, specific adjustments to correct atlas and axis misalignment.
Unlike forceful adjustments that involve twisting or "cracking" the neck, Blair corrections are applied as precise, controlled pressure to move the vertebra back toward its optimal position.
Key principles of Blair upper cervical care include:
- Precision analysis: Three-dimensional x-ray analysis identifies the exact direction and degree of misalignment
- Individualized correction: Each adjustment is tailored to the person's unique anatomy and specific misalignment pattern
- Gentle force: Light pressure (often just 1-5 pounds of force) rather than high-velocity thrusting
- Hold time: After correction, the body is given time to stabilize, with fewer adjustments needed as alignment improves
Treatment Protocol
A typical upper cervical treatment plan for vertigo includes:
Initial Phase (First 2-4 Weeks):
- Comprehensive evaluation and precision imaging
- Initial atlas correction
- Frequent monitoring to ensure the adjustment is holding
- Typical visit frequency: 2-3 times per week initially
Stabilization Phase (Weeks 4-12):
- Progressive reduction in visit frequency as alignment stabilizes
- Re-imaging to document correction maintenance
- Adjustments only when objective testing shows misalignment
- Visit frequency: Once weekly, then bi-weekly
Maintenance Phase (3+ Months):
- Periodic check-ups to maintain optimal alignment
- Adjustments only when needed, not on every visit
- Focus on lifestyle factors that support spinal health
- Visit frequency: Monthly or as-needed basis
What Makes Upper Cervical Care Different
Unlike vestibular rehabilitation therapy or medications that manage symptoms, upper cervical care addresses a potential underlying cause.
Rather than treating vertigo as an inner ear problem exclusively, this approach recognizes that cervical spine alignment can directly influence vestibular function.
The goal isn't temporary symptom relief but correction of the underlying structural problem. When the atlas and axis are properly aligned, normal nerve communication is restored, proprioceptive input becomes accurate, and the vestibular system can function as designed.
Upper cervical chiropractors may recommend complementary approaches:
- Specific exercises to support cervical stability
- Posture correction strategies
- Ergonomic modifications for work and sleep
- Hydration and nutritional support
- Stress reduction techniques
- What to Expect During Care {#what-to-expect}
- Understanding the upper cervical care process helps set appropriate expectations and maximize treatment benefits.
First Visit (60-90 minutes):
Your initial consultation includes a thorough health history review, comprehensive examination, and discussion of your vertigo symptoms and their impact on your life.
The chiropractor will perform neurological and orthogonal tests to identify upper cervical involvement.
If imaging hasn't been done recently, specialized x-rays will be taken. These aren't standard neck x-rays, they're precise Blair protocol views that show the exact position of your atlas and axis in three dimensions.
Second Visit (30-45 minutes):
The chiropractor reviews your x-rays, explaining your specific misalignment pattern and how it may be contributing to your vertigo. If appropriate, your first upper cervical correction is performed.
The actual adjustment is gentle and controlled. You'll lie on a specialized table, and the chiropractor applies light, sustained pressure to move the atlas in the precise direction needed. There's typically no twisting, popping, or cracking involved.
Immediate Post-Adjustment:
After the correction, you'll rest briefly to allow your body to process the change. Some people notice immediate improvement in symptoms, while others experience gradual changes over several days or weeks.
It's not uncommon to feel somewhat tired or have mild soreness after the first few adjustments as your body adapts.
Follow-Up Visits:
Initially, visits are frequent (2-3 times weekly) to monitor whether the correction is holding. The chiropractor performs objective tests each visit to determine if another adjustment is needed—not every visit includes an adjustment. As your spine stabilizes, visit frequency decreases.
Progress Timeline:
- Weeks 1-2: Focus on holding the initial correction; symptoms may fluctuate
- Weeks 3-6: Increasing stability; many patients notice vertigo episodes becoming less frequent or severe
- Weeks 7-12: Continued improvement; most patients experience significant symptom reduction 3-6
- Months: Stabilization phase; maintenance schedule established
Factors Affecting Results:
- Injury severity and chronicity: Recent injuries often respond faster than decades-old misalignments
- Overall health status: General health influences healing capacity
- Compliance: Following care recommendations improves outcomes
- Lifestyle factors: Stress, sleep quality, and physical activity all play roles
- Concurrent conditions: Other health issues may slow or complicate recovery
Success Rates and Research
Evidence supporting upper cervical chiropractic care for vertigo comes from clinical studies, case reports, and documented patient outcomes.
Research Findings:
A 2019 study published in the Journal of Upper Cervical Chiropractic Research found that 77% of patients with cervicogenic vertigo experienced significant improvement with Blair upper cervical care, with 42% achieving complete resolution of symptoms within 12 weeks.
Research from 2020 examining post-concussion vertigo found that upper cervical chiropractic adjustments, when combined with vestibular rehabilitation, produced better outcomes than vestibular therapy alone, with 68% of patients reporting substantial improvement compared to 43% in the control group.
A comprehensive review of cervicogenic dizziness published in 2021 concluded that manual therapy targeting the upper cervical spine showed promising results, particularly for vertigo associated with neck pain or history of cervical trauma.
Clinical Outcomes:
Upper cervical practitioners consistently report that patients with certain characteristics respond particularly well:
- Recent trauma history (6 months to 5 years): 70-85% significant improvement
- Chronic post-concussion symptoms: 60-75% improvement
- Vertigo with neck pain: 65-80% improvement
- Failed inner ear treatments: 55-70% improvement with upper cervical care
Realistic Expectations:
Not every vertigo case is caused by upper cervical misalignment, and not everyone who has misalignment will experience complete resolution.
However, many patients report significant quality of life improvements even if some mild symptoms persist.
Results are typically most dramatic for:
- Cervicogenic vertigo
- Post-traumatic vertigo
- Vertigo associated with neck pain
- Dizziness that worsens with head/neck movement
Upper cervical care may provide some benefit even for inner ear conditions like Ménière's disease, though results are more variable. The rationale is that optimal upper cervical alignment supports overall neurological function, potentially helping the body compensate more effectively.
Long-Term Outcomes:
Follow-up studies indicate that patients who achieve good initial results with upper cervical care tend to maintain those improvements long-term, especially when they return for periodic maintenance care.
The key is establishing and maintaining proper alignment rather than repeatedly treating symptoms.
When to Seek Upper Cervical Care
Certain patterns strongly suggest that upper cervical chiropractic evaluation would be beneficial for your vertigo.
Consider scheduling a consultation if you have:
- History of neck trauma: Auto accidents, falls, sports injuries, or concussions, even from years ago
- Vertigo + neck pain: Dizziness accompanied by neck pain, stiffness, or reduced range of motion
- Position-dependent symptoms: Vertigo that's triggered or worsened by specific neck positions
- Failed conventional treatments: Little or no improvement from medications, Epley maneuvers, or vestibular rehabilitation
- Post-concussion syndrome: Persistent dizziness following head injury
- Chronic headaches with vertigo: Especially headaches originating from the base of the skull
Red Flags Requiring Medical Evaluation First:
Before pursuing upper cervical care, rule out serious conditions if you have:
- Sudden severe vertigo with neurological symptoms
- Vertigo with hearing loss or facial weakness
- Symptoms suggesting stroke or transient ischemic attack
- Severe, progressively worsening symptoms
- Loss of consciousness or seizures
Appropriate Expectations:
Upper cervical care is not a quick fix or emergency treatment. It's a systematic approach to correcting underlying structural problems that may be causing or contributing to vertigo. Most patients need several weeks of care before experiencing significant, lasting improvement.
If you're experiencing acute, severe vertigo, seek immediate medical evaluation to rule out conditions requiring urgent intervention.
Once serious causes are excluded, upper cervical evaluation becomes appropriate, especially if you have risk factors or characteristics suggesting cervicogenic involvement.
Frequently Asked Questions
1. How long does it take to see results from upper cervical care for vertigo?
Most patients begin noticing changes within 2-4 weeks of starting care, though the timeline varies based on how long the misalignment has been present and the severity of symptoms.
Acute cases (recent injuries) often respond faster than chronic conditions that have persisted for months or years.
Typical progression includes initial fluctuation of symptoms during the first 1-2 weeks as the body adjusts, followed by gradual improvement in vertigo frequency and intensity. Significant improvement usually occurs within 6-12 weeks of consistent care.
If you're experiencing severe, debilitating vertigo that's preventing daily activities, schedule an evaluation within the next few days rather than waiting to see if symptoms resolve on their own.
2. Is upper cervical chiropractic safe for treating vertigo?
Blair upper cervical technique is considered one of the gentlest forms of chiropractic care. The adjustments use minimal force and don't involve the twisting or high-velocity movements associated with traditional chiropractic adjustments. Serious complications are extremely rare.
However, a thorough evaluation is essential to ensure upper cervical care is appropriate for your specific condition. The precision imaging and careful assessment that characterize Blair technique help ensure safety.
If you've been diagnosed with vertebral artery problems, severe osteoporosis, or certain spinal conditions, inform your upper cervical chiropractor before beginning care, as these may require modified approaches or contraindicate certain techniques.
3. Can upper cervical adjustments cure all types of vertigo?
No single treatment cures all types of vertigo because vertigo has multiple potential causes. Upper cervical care is most effective for cervicogenic vertigo, dizziness originating from neck problems. It may also provide benefit for some cases of post-concussion vertigo and vestibular dysfunction where upper cervical misalignment is a contributing factor.
Inner ear conditions like BPPV or Ménière's disease have different primary causes and typically require different interventions, though some patients with these conditions experience improvement with upper cervical care as a complementary approach.
The key is accurate diagnosis to determine whether upper cervical involvement is present. Schedule a comprehensive evaluation that includes both medical and upper cervical assessment to determine the best treatment approach for your specific type of vertigo.
4. How is Blair upper cervical different from regular chiropractic?
Blair technique differs in several key ways: it focuses exclusively on the atlas and axis vertebrae rather than adjusting the entire spine; it uses precision three-dimensional x-ray analysis to measure exact misalignment; it employs gentle, specific corrections rather than general manipulations; and adjustments are performed only when objective testing confirms misalignment is present, not on every visit.
General chiropractic care often includes multiple spinal regions and may use techniques that involve more forceful adjustments with audible "cracking."
Blair technique uses controlled, sustained pressure without rotation or thrusting. The philosophy centers on correcting the primary misalignment (the atlas) and allowing the body's innate intelligence to restore optimal function throughout the spine.
5. Will I need upper cervical adjustments forever?
The goal of upper cervical care is to achieve lasting correction, not create dependence on continuous treatment. Initially, frequent visits help establish and stabilize the correction. As your spine stabilizes, adjustments are needed less frequently.
Many patients transition to a maintenance schedule of monthly or periodic check-ups once optimal alignment is achieved. The frequency of maintenance care varies based on lifestyle factors, stress levels, physical demands, and how well your body maintains alignment.
Some patients maintain good alignment for months between adjustments, while others benefit from more frequent monitoring. The ideal approach is periodic evaluation to detect and correct any misalignment before symptoms recur, similar to dental check-ups that prevent problems rather than just treating them after they develop.
6. What should I do if vertigo returns after upper cervical treatment?
If vertigo symptoms return after experiencing improvement, contact your upper cervical chiropractor for re-evaluation. Symptoms can recur if the atlas misaligns again due to trauma, stress, poor sleeping positions, or accumulated postural strain.
Re-examination will determine whether the atlas has shifted out of alignment or if symptoms are due to other factors. If misalignment is present, a correction can be performed. If alignment has remained stable, other contributing factors may need to be addressed.
Some patients experience temporary symptom fluctuations during the healing process before achieving long-term stability. Schedule a follow-up appointment within 3-5 days of symptom recurrence rather than waiting to see if it resolves, as early correction often prevents symptoms from becoming re-established.
7. Can upper cervical care help if I've had vertigo for years?
Yes, even chronic vertigo that has persisted for years can improve with upper cervical care if atlas or axis misalignment is a contributing factor.
While chronic cases often take longer to respond than recent onset vertigo, many patients experience significant improvement regardless of how long they've had symptoms.
The key factors are whether upper cervical misalignment is present and whether other complications have developed over time. Comprehensive evaluation, including precision imaging, determines if upper cervical involvement exists and estimates the likelihood of improvement.
Chronic cases may require a longer treatment period and more adjustments to achieve stability, but substantial symptom reduction is possible. Don't let the duration of your symptoms discourage you from seeking evaluation, many people with years of unsuccessful treatments find relief through upper cervical care when the underlying cause is finally addressed.
Do I Need to See a Doctor? Self-Assessment
Answer these questions honestly about your vertigo symptoms:
- Do you have a history of head or neck injury (car accident, fall, sports injury, concussion)?
- Does your vertigo worsen with certain neck positions or movements?
- Do you experience neck pain, stiffness, or headaches along with vertigo?
- Have conventional treatments (medications, Epley maneuver, vestibular therapy) provided little or no relief?
- Is your vertigo interfering with daily activities, work, or driving?
- Do episodes of vertigo last more than a few seconds or occur frequently?
- Are you experiencing additional symptoms like visual problems, difficulty concentrating, or persistent nausea?
- Has your vertigo persisted for more than two weeks?
Your Results:
0-1 "Yes" answers: Your symptoms may be mild or intermittent. Monitor symptoms and practice self-care measures. If symptoms persist beyond 2 weeks or worsen, schedule an evaluation.
2-3 "Yes" answers: Professional evaluation recommended within 1-2 weeks. Your symptoms suggest a pattern that warrants upper cervical assessment, especially if you have a history of neck trauma or neck pain with vertigo.
4-5 "Yes" answers: Schedule an appointment within 2-3 days. Multiple indicators suggest upper cervical involvement in your vertigo, and prompt evaluation can help prevent symptom worsening and identify the underlying cause.
6+ "Yes" answers: Contact an upper cervical chiropractor this week. Your symptom pattern strongly suggests cervicogenic vertigo or post-traumatic dysfunction that could significantly benefit from specialized care. Don't continue suffering—upper cervical evaluation is warranted.
Seek Emergency Medical Attention If You Experience:
- Vertigo with sudden severe headache ("worst headache of your life")
- Weakness, numbness, or difficulty moving one side of your body
- Slurred speech or difficulty speaking
- Vision loss or severe visual disturbances
- Loss of consciousness
- Chest pain or difficulty breathing
- Signs of stroke (facial drooping, arm weakness, speech difficulty)
Ready to Take the Next Step?
Sarasota Upper Cervical Chiropractic
Remember: Vertigo doesn't have to be a life sentence. If you suspect upper cervical involvement—especially if you have a history of neck trauma or failed conventional treatments—specialized evaluation may provide the answers and relief you've been seeking.
Vertigo is a complex condition with multiple potential causes, but upper cervical spine misalignment is an often-overlooked contributor that can be effectively addressed with specialized chiropractic care.
The Blair technique offers a precise, gentle approach that corrects atlas and axis misalignment, potentially restoring normal vestibular function and eliminating vertigo at its source.
Research supports that 60-85% of patients with cervicogenic vertigo experience significant improvement with upper cervical care, particularly when there's a history of neck trauma, symptoms worsen with neck movement, or conventional treatments have failed.
While not a cure-all for every type of vertigo, this specialized approach addresses an underlying structural problem that mainstream treatments often miss.
The key is accurate diagnosis. If your vertigo includes neck pain, follows head or neck trauma, or hasn't responded to inner ear treatments, upper cervical evaluation is warranted. Early intervention often produces better results than waiting until symptoms become severe or chronic.
Don't accept vertigo as an inevitable part of your life. If the upper cervical connection resonates with your experience, specialized evaluation may provide the breakthrough you've been seeking.
Upper cervical misalignment can cause or contribute to vertigo by disrupting the vestibular system, brainstem function, and cervical proprioception. The Blair technique uses precision imaging and gentle corrections to restore proper atlas and axis alignment without forceful manipulation
Success rates of 60-85% are reported for cervicogenic vertigo, with best results in patients who have neck trauma history or neck-related symptoms. Most patients notice improvement within 4-8 treatment sessions, though chronic cases may require longer care
Upper cervical care addresses the underlying cause rather than just managing symptoms, offering potential for lasting resolution rather than temporary relief
References
Hain, T.C., & Uddin, M. (2020). Cervical vertigo: a review of diagnosis and treatment. Journal of Vestibular Research, 30(3), 175-186.
Burcon, M.T. (2019). Upper cervical protocol and results for 139 patients with medically diagnosed Meniere's disease. Journal of Upper Cervical Chiropractic Research, 2019(2), 1-12.
Marshall, C., et al. (2020). The effectiveness of upper cervical chiropractic care on dizziness and balance disorders: a systematic review. Journal of Manipulative and Physiological Therapeutics, 43(5), 463-473.
Reid, S., & Rivett, D. (2021). Manual therapy for cervicogenic dizziness: a systematic review. Manual Therapy, 16(1), 4-13.
Hawk, C., Cambron, J.A., & Pfefer, M.T. (2021). Cervicogenic vertigo: diagnosis and treatment approaches. Chiropractic & Manual Therapies, 29(1), 28-41.
Schubert, M.C., & Minor, L.B. (2020). Vestibulo-ocular physiology underlying vestibular hypofunction. Physical Therapy, 90(9), 1310-1320.
Brandt, T., & Dieterich, M. (2019). Vertigo and dizziness: common complaints. New England Journal of Medicine, 380(10), 956-965.
Malmström, E.M., et al. (2020). The role of cervical afferent information in dizziness and unsteadiness following whiplash injury. Journal of Rehabilitation Medicine, 52(7), jrm00074.
Woodhouse, A., & Vasseljen, O. (2021). Altered motor control patterns in whiplash and chronic neck pain. BMC Musculoskeletal Disorders, 9, 90-102.
Treleaven, J. (2020). Dizziness, unsteadiness, visual disturbances, and postural control: implications for management of patients with neck pain. Journal of Orthopedic & Sports Physical Therapy, 40(8), 492-502.
Hsieh, C., Phillips, R.B., et al. (2019). Functional outcomes of low back pain: comparison of four treatment groups in a randomized controlled trial. Spine, 44(15), 1050-1060.
Lystad, R.P., Bell, G., Bonnevie-Svendsen, M., & Carter, C.V. (2021). Manual therapy with and without vestibular rehabilitation for cervicogenic dizziness: a systematic review. Chiropractic & Manual Therapies, 29(1), 19-34.





Leave a comment